From the Mayo Clinic
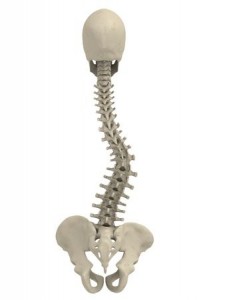
Scoliosis is the development of asymmetrical curvature and twisting of the spine. It’s commonly thought of as a disease that occurs in adolescents, and is sometimes associated with wearing a back brace to keep the curve from worsening.
In fact, scoliosis is more common in older adults than in adolescents. Some adults who had scoliosis as adolescents may see gradual worsening of their scoliosis with age, but the majority of older adults with scoliosis didn’t have it earlier in life.
Scoliosis in older adults is a distinctly different problem from that in adolescents. In adults, back braces are used sparingly, if at all. Adults often benefit most from regular exercise. If surgery is needed, breakthroughs have made certain scoliosis procedures far easier on the body and far more effective than in the recent past.
What’s happening?
Scoliosis in older adults is usually caused by the wear and tear (degeneration) of the spine that commonly occurs with age. This may include back problems such as:
Degenerating disks — Disks are the pads between your vertebrae that act as cushions and allow for spine flexibility. Disk degeneration is a natural part of aging, and diminished disks can place more pressure on joints of the spine. When a disk degenerates unevenly, eventually scoliosis can result.
Osteoporosis — This weakening and thinning of bone can cause the vertebrae to fracture and compress. Asymmetric compression can contribute to scoliosis.
Prior back surgery that removed spine tissues — Procedures such as laminectomy or facetectomy that remove parts of the spine that are pressing on nerves can lead to spine imbalance.
Arthritis — Specifically, this is the development of wear-and-tear (osteoarthritis) in the joints of your spine (facet joints). Spine imbalance — whether caused by pre-existing curvature from youth, disk degeneration or osteoporosis-related degeneration — places uneven force on facet joints. This can cause or worsen arthritis in those joints, leading to further imbalance of the spine.
Pain progression
Scoliosis in older adults isn’t necessarily considered a problem until symptoms develop. Most older adults with considerable spinal curves — especially those who are fit and healthy — can be quite active with no symptoms at all.
Problems with scoliosis are often preceded by lack of fitness — specifically the loss of strength in the core muscles of the trunk — and being overweight or obese. These factors — in addition to spine degeneration and unbalanced spinal mechanics — may at first cause low back pain. Over time, osteoarthritis of spine joints may develop or worsen. The body responds by producing bony outgrowths that can pinch or compress root nerves that branch from the main spinal column. This can lead to pain or numbness that radiates down one leg and may cause leg weakness. The pain may come and go.
The body also responds by thickening spine ligaments. These can gradually squeeze or compress your spinal column (spinal stenosis). It may take years, but this may cause pain that’s centered in the buttocks, rather than radiating down the leg. Position changes such as sitting and leaning forward can often provide relief. But as ligament thickening progresses, position changes provide less relief and leg weakness may make it difficult to walk.
Stooped posture is another concern with scoliosis. To relieve pain, you may tip your trunk forward while standing or walking. This can strain and fatigue back muscles, or even cause painful muscle spasms. Additional concerns may include having a rib that pinches against the pelvis or compression of abdominal organs, particularly in those who are overweight. Advanced scoliosis may even make it difficult to keep yourself upright.
Get active
Usually, treatment of pain from degenerative scoliosis is similar to treatment for other types of chronic back pain. Strategies include:
Exercising — Exercise, such as yoga or Pilates, that strengthens core muscles of the trunk is one of the biggest determinants of long-term health. Avoid extremes of rotation and bending, and use good posture. Balance training and overall fitness can help prevent falls.
Load-bearing exercise such as walking can help combat bone degeneration. Aquatic exercise may be a good alternative if walking is too difficult or painful.
Addressing bone health — Work with your doctor to develop a plan to stop or slow bone thinning that can lead to osteoporosis and increase risk of spine fractures. This includes getting adequate calcium and vitamin D and possibly taking osteoporosis medications.
Maintaining a healthy weight — The more weight you carry, the more stress it puts on your back.
Stopping smoking — Smoking reduces blood flow to disks and accelerates disk degeneration.
Using pain therapies — Acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin, others) or naproxen (Aleve, others) can help relieve pain. Certain antidepressants and anti-seizure drugs also may be considered. Your doctor may prescribe narcotic-containing drugs for severe, persistent pain.
If inflammation and swelling around nerves is a suspected component of your pain, an injection of an inflammation-reducing corticosteroid drug may help provide pain relief that can last for a few months.
Surgery that helps
Regardless of the severity of scoliosis you have, surgery won’t help you if you still have good balance, manageable pain and are able to function. However, surgery may be indicated when you have:
Radiating nerve root compression that’s also causing leg weakness or significant disability
Compression of the spinal column that’s causing pain and weakness, especially if the pain doesn’t subside with an injection of an inflammation-reducing corticosteroid or other pain therapies
Since nerve compression and pinching are the main indications for surgery, surgery often involves removing tissues — such as bone or disk material — that are pressing on a nerve and causing pain or other symptoms. When this nerve decompression involves removal of facet joint tissue (facetectomy), it may cause or worsen spine instability. Therefore, your surgeon may couple this with additional work to fuse spine segments together or implant metal bracing devices to add stability to the spine.
In the past, fusing vertebrae often involved harvesting bone from the pelvis, requiring more incisions, blood loss, pain and hospitalization. Even then, the fusion failed about a third of the time and most people ended up with ongoing pain where bone was harvested.
Today, traditional bone fusion is done less frequently in scoliosis surgery. Synthetic fusion options may include the use of bone morphogenetic protein (BMP). This naturally occurring growth factor stimulates bone growth.
Surgeons soak a small collagen sponge in a BMP-infused liquid. The sponge is then placed within spinal segments, where it stimulates rapid bone growth that spreads from natural bone and permeates the sponge. Within months, the sponge is replaced by bone.
At Mayo Clinic, BMP fusions can reduce blood transfusion needs in large scoliosis procedures by about 80 percent. Hospital stays can be reduced from five to seven days to two to three.
However, it’s not an option for people with existing tumors, as the growth factor may accelerate tumor growth. There’s controversy as to whether BMP increases cancer risk in those without tumors, but Mayo Clinic experts believe the risk — if any — is very low.
Fusion with BMP may eliminate the need to take bone from elsewhere. The rate of successful fusion is consistently greater than 90 percent, often enabling spinal fusion procedures to be done through much smaller incisions.
At Mayo Clinic, BMP fusions can reduce blood transfusion needs in large scoliosis procedures by about 80 percent. Hospital stays can be reduced from five to seven days to two to three.
At Fit N Pilates located in North Dallas in Plano Texas, we specialize on the core exercises that help relieve symptoms associated with scoliosis.